Going home from the hospital after cardiac surgery

Information and resources for returning home from cardiac surgery.

This video has subtitles in multiple languages. To access them, click on the wheel icon (settings) at the bottom right of the video player, click “Subtitles,” and then choose from the list of languages.
What to expect
Everybody recovers at a different rate depending on their general health, any pre-existing health conditions, and the type of surgery.
Generally, you are ready to leave the hospital when:
- Your blood pressure, heart rate, temperature, and blood tests are normal for you.
- Your incision is healing.
- Your abdomen is soft and not bloated.
- You have bowel activity (passing gas or having bowel movements).
- You can manage your pain with oral pain pills.
- You are eating well enough.
- You can walk short distances.
- You can look after yourself and do simple self-care at home (with help if needed).
- You can look after yourself at home (with help if needed).
- If you still have sutures (stitches) or staples still in place when you are discharged, you will need to go to your primary care provider to have them removed. The health-care team will advise you when to get them removed. Ask the health-care team if you have any other questions.
Your ride home
- When it is determined you are ready to go home, please arrange for a ride.
- The day before you go home, confirm with the health-care team what time your ride should come and get you from the unit.
- If you cannot get picked up by the time recommended by the health-care team, we may ask you to wait in the Patient Lounge. We do this so we can get your bed cleaned and ready for the next patient.
- If there is a problem getting a ride or getting home, you may need to stay in a local hotel. Discuss any problems you may have with the health-care team. You cannot continue to stay in the hospital if we feel you are well enough to leave.
Information you will get when you leave the hospital
You will receive discharge teaching during your hospital stay. If you have questions please ask your nurse. When you leave the hospital, you will be given a discharge package containing important information.
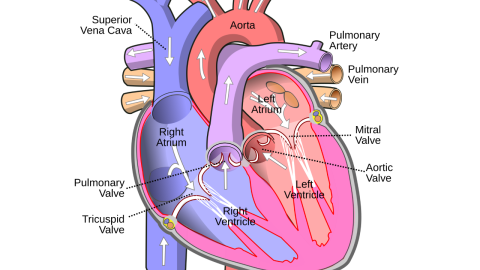
If you had CABG surgery, you will receive a diagram of your heart vessels that shows where the bypass grafts were placed.
If you had valve surgery, you will receive a temporary valve card: please keep this in your wallet. A permanent card will be mailed to your home in a few months.
Please bring this information to all your follow-up appointments.
Health equipment
While you are in the hospital, the occupational therapist and/or physiotherapist may determine you require some equipment to be independent and safe while you continue to recover at home. If this is the case, you will receive a prescription from the occupational and/or physiotherapist to borrow equipment from the Red Cross.
You, a family member, or a friend must pick up the equipment. You can phone ahead to reserve the equipment. Most people arrange for a family member or friend to pick up the equipment on the days before or the day of discharge.
Please be aware that some locations are not open on weekends, and equipment may need to be picked up ‘early’ in case you are discharged on a weekend. The number for the Red Cross can be found at the bottom of this page.
Follow-up visits
Before you go home, a health-care team member will discuss your plan for follow-up with your primary care provider and surgeon.
Typically the following will be suggested:
- Primary Care Provider in one week.
- Cardiologist in six to eight weeks.
- Cardiac Surgeon within three months.
- Cardiac Rehabilitation referral
The health-care team may also provide you with the following if needed:
- A prescription for medication
- A form for blood tests
- Cardiac Rehabilitation Program information
The Care Management Leader (CML) refers all patients to the Cardiac Rehabilitation Program (may also be called the Healthy Heart Program) in their community. This program often includes cardiac education, supervised exercise, nutrition counselling, and psychosocial support. It usually begins two to three months after you are discharged from the hospital from your surgery.
There may be online and in-person classes available, depending on the location you attend. An associated cost may be applicable to attend the program.
Medications
Your health-care team may send you home with some medications. You will be given a prescription and will be responsible for filling it from a drugstore. A health-care team member will review your medications with you. Remember to take them as ordered and ask the health-care team or your pharmacist if you have any questions.
You will also be told whether you need to continue with your previous medications and when to restart them. If you are not told by the time you are discharged home, ask your primary care provider.
Please do not stop or change your medications on your own. Your primary care provider may change, re-order or stop them for you. Please do not take any other medicines or “over-the-counter” remedies unless you have checked with your primary care provider.
Ask your health-care team for information sheets about your medications.
Please ask the health-care team and/or primary care provider before taking any herbal or traditional medications (some can cause a risk of bleeding).
Alcohol can have negative side effects with certain medications. Always read and follow any instructions provided with your medications.
Blood thinners
Anticoagulant medications are often called “blood thinners”. They do not really “thin” the blood. Instead, they stop blood from clotting as fast as it usually does. Anticoagulants increase the risk of bleeding. If you are started on an anticoagulant, this is because the benefits of being on a blood thinner (to prevent or treat a clot) outweigh the risks associated with being on a blood thinner (bleeding). You might be on an anticoagulant if you have an artificial heart valve, valve repair, or atrial fibrillation (an irregular heart rhythm). Depending on which anticoagulant you are taking, you may have to go for frequent blood tests (i.e. once weekly at the beginning) for the first 3 months to monitor the “thinness” of the blood.
If you develop unexplained bruising, blood in your urine or stool, or start coughing up blood, contact your health-care team or primary care provider or go to the Emergency Department.
People who take anticoagulant medication for a long time are advised to wear a MEDIC-ALERT bracelet. Ask your primary care provider about this.
Water pills
If the health-care team asks you to take a water pill at home, please weigh yourself daily. Try to do this each morning after you go to the bathroom and before you get dressed.
Record your weight. Gaining four pounds (two kilos) in two days or five pounds (two and a half kilos) in one week might be due to extra body fluid. If you notice this sudden weight gain, please call your primary care provider. If you notice swelling in your ankles, you should also call your provider.
Emotions and feelings
You and your family members or friends may feel a range of emotions going home. You may feel excited, relieved, scared, worried or “blue” (in low spirits). This is common. You may find sharing and discussing your concerns with your health-care team helpful. Be assured that the health-care team will only discharge you if you are medically ready.
When to get help
Contact your surgeon or primary care provider or go to the Emergency Department if any of the following happens:
- Your pain gets worse or does not go away with pain medication.
- You have a fever over 38.0° C (100.4° F).
- Your incision comes apart or becomes red, swollen, or hot to the touch.
- You notice foul-smelling liquid coming from your incision.
- You start bleeding from your incision.
- You have difficulties with swallowing, resulting in a decreased appetite and constant weight loss.
- You feel sick to your stomach (nauseated) or throw up (vomit) often for more than 24 hours.
- You have diarrhea that lasts for more than two days.
- If you experience any pain, aching or redness in your calves and/or swelling of the legs.
- You have difficulty breathing.
If you cannot contact your surgeon or primary care provider, go to the nearest Emergency Department or call HealthLink BC at 8-1-1 to talk to a registered nurse. Be sure to tell them about your recent surgery.
Resources
-
-
Red Cross
-
Red Cross Lower Mainland HELP Locations
-
Recovery and support
-