Your recovery in hospital after cardiac surgery

This page describes what you can expect to see and feel while recovering in hospital. Recovery can take a lot out of you, and everyone's recovery is different.
What to expect: your surgical journey
Each person’s recovery is different. Depending on the type of surgery, most people are ready to go home in four to seven days.
Cardiac Surgery Intensive Care Unit (CSICU)
When your surgery is finished, you will be moved to the Cardiac Surgery Intensive Care Unit (CSICU). You will wake up in the CSICU and may feel drowsy. You may see other patients nearby as they have had similar operations.
You might have some or all of the following:
-
Endotracheal (Breathing) Tube
This tube is put through your mouth into your windpipe and attached to a breathing machine called a ventilator. This machine breathes for you during and after surgery until you can breathe strongly on your own again. When you first wake up, this tube will still be in your throat. It may feel uncomfortable but know it will be removed as soon as you can breathe on your own (about three-12 hours after the surgery).
-
Foley catheter
This is a tube that will drain urine from your bladder. You may have the urge to urinate while the catheter is in place. This will be removed one to two days after your surgery when you are able to use a bedside urinal or go to the toilet.
-
Intravenous (IV) lines
You will have an intravenous (IV) line inserted into a vein in your neck to deliver medications and assess blood flow and pressure in your heart. This is called a central line. It will be removed when it is no longer needed.
You will also have an IV line in your arm, which will stay in place until you have been in the ward for a few days.
-
Chest drainage tubes
Chest drainage tubes are placed in your chest near the bottom of your incision during surgery. They drain blood and fluid that collects in your chest after surgery. They are usually removed the day after your surgery. Some patients find this uncomfortable. Pain medication will be given before removal to make you more comfortable.
-
Temporary pacemaker wires
You may also have temporary pacemaker wires inserted at the time of surgery. These are purple wires with metal tips placed on the surface of your heart and brought out to the surface of your chest. These wires allow staff to attach an external pacemaker if they need to improve your heartbeat. You will not be able to feel this. The wires will be removed once your heart is in a stable rhythm. This usually occurs close to your discharge date.
The CSICU nurse will:
- Check your blood pressure, pulse, and breathing rate.
- Check your bandage (or dressing).
- Ask you about your pain and nausea.
- Encourage you to start your deep breathing exercises.
Once you can breathe on your own without the assistance of the breathing machine (mechanical ventilator), the breathing tube is removed. This usually occurs within four to six hours of waking up.
You will stay in the CSICU for one or two nights until you are well enough to be cared for in the surgical nursing unit (LB10A) and a bed is available. Once you are transferred to the unit, your family and friends can visit you. In the CSICU, you can have one immediate family member or friend visit you at a time.
Surgical Nursing Unit (LB10A)
While you are in the Cardiac Sciences Acute Care Unit, your health-care team’s goals are:
- Manage your medical conditions
- Control your pain and prevent problems during your recovery
- Increase your activity to help build your strength
- Ensure you are eating enough
-
Prepare you to go home
Most people will stay on the unit for three to four days (totaling five to seven days after their surgery), but this depends on the type of surgery and your health. The health-care team will keep you informed of your progress and when you are expected to leave the hospital.
On LB10A, you will be in a room and will continue to be monitored and receive care by the health-care team. Family or support people can visit but may not stay at the hospital during your stay. Talk to the nurse if you have questions or concerns about getting support.
Please speak with your health-care team if you would like to request any of the following:
- Virtual Interpreter services, if your first language is not English
- Indigenous Health services
Medications
We understand that you may have been taking certain medications before your hospital stay that are not available in our pharmacy.
During your hospital stay, it's important that you only take medications that are prescribed by the health-care team and provided by the nursing staff.
To avoid any unexpected harmful combination of medications, please be aware of the following:
- If you are taking a medication that is not available from our pharmacy, you may be given an alternative or asked to bring your own personal supply of medication to use while you are in the hospital.
- The nursing staff will keep the medication in a safe place and provide you with the medication at the prescribed time, as per the provider.
- Any unused medication you bring to the hospital will be returned to you before you go home.
Handwashing
Washing your hands is the most important and effective way to prevent the spread of infection and to protect yourself and your loved ones.
There are two ways to clean your hands:
- You may wash at the sink using soap and water – put soap on your hands and rub your hands for a total of 30 seconds. Rinse with warm water. For more information on hand hygiene, view our how to handwash poster.
- You may use the alcohol-based hand sanitizer throughout the hospital — take one squirt, rub it over your hands for 30 seconds and allow it to dry.
It is important to wash your hands:
- After using the washroom.
- Before eating.
- When entering and leaving your room.
It is okay to ask staff and visitors to wash their hands.
Pain control
Many people are concerned about pain after their surgery. Some people try to “grin and bear" their pain, while others do not want to take pain medication because they are concerned about becoming addicted or constipated. When you take opioid medication for acute pain, such as the pain that happens after operations or accidents, the risk of addiction is low.
Adequate pain control is important to your recovery. Having your pain under control allows you to:
- Breathe deeply to prevent lung infections.
- Move to prevent blood clots.
- Sleep well.
- Eat better for wound healing.
- Recover faster.
Several different pain medications will be given regularly. These pain medications will help reduce the amount of opioids required. You will receive these pain medications even if you are not in pain at the time. If you are asleep, the nurse will wake you to take these regular medications.
- You will get acetaminophen (Tylenol) four times a day throughout your stay (maximum two to four grams per day, depending on your medical conditions).
- You will get other pain medications as needed.
Non-medication therapy to help ease the pain
For additional pain control, you may also want to add:
- Listening to music.
- Doing slow and relaxed breathing.
- Moving around and positioning.
- Imagining peaceful situations.
Pain management
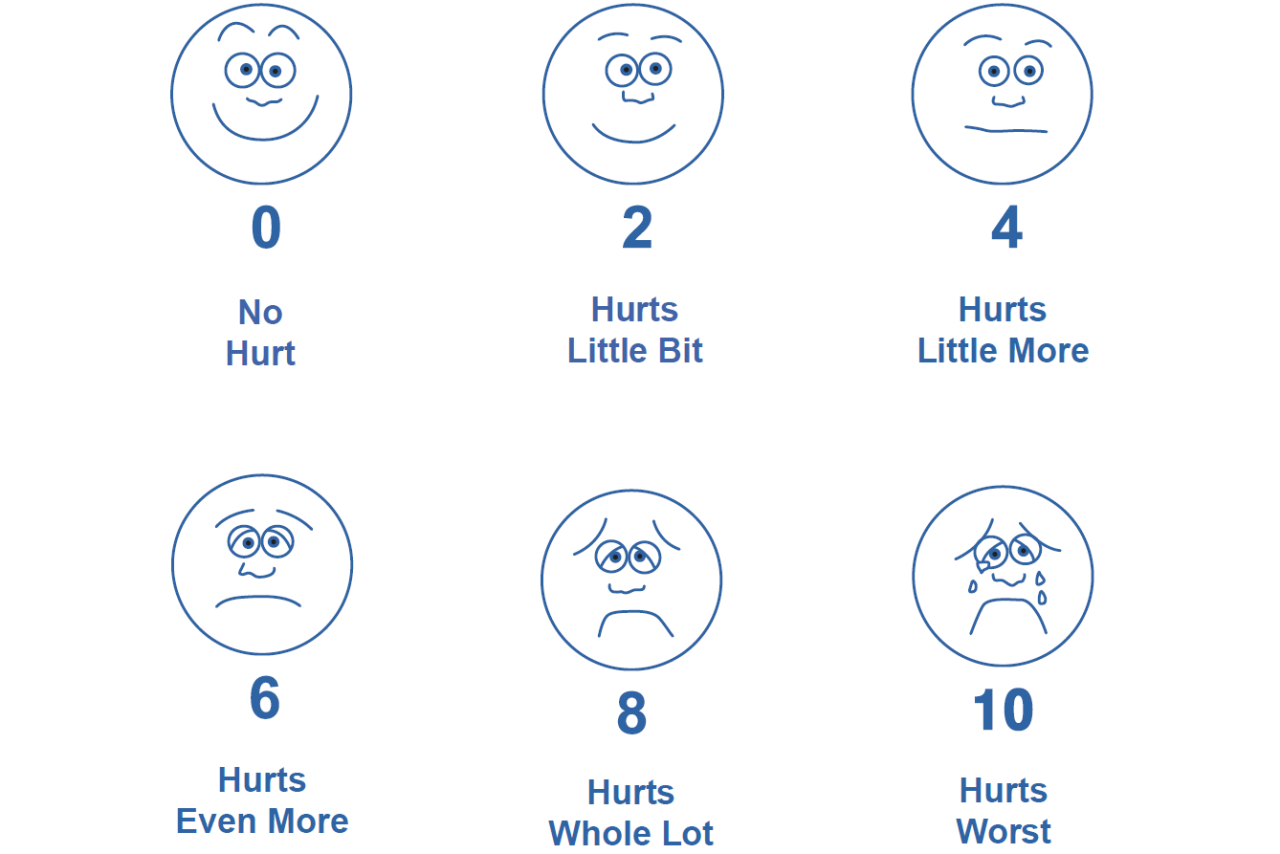
An important part of managing pain is monitoring how much pain you are having. The best way to monitor your pain over time is to use something to measure the amount of pain you have.
We use a pain rating scale to help us assess your pain/discomfort and the effectiveness of the pain medication. We will ask you to rate your pain/discomfort on a scale of 0-10, where 0 means no pain/discomfort at all, and 10 is the worst pain/discomfort ever.
We want your pain to be:
- At 0, 1, 2, or 3 on the number scale, or
- At an acceptable level, so you can carry out your normal activities, such as washing up, sitting, and walking.
*Pain medication works best if it is taken BEFORE the pain becomes uncomfortable.*
Knowing that pain medication will not make your recovery pain-free is important. The goal is to manage your pain and to help you resume your regular activities.
Let your nurse know if your pain does not get better with pain medication or is getting worse.
Nausea and vomiting
It is common to feel sick to your stomach or throw up after surgery. If you feel nauseated or are vomiting, avoid drinking large amounts of fluid.
Let your nurse know as soon as you feel sick to your stomach. The nurse can give you medication to help you feel better and prevent it from worsening.
Other ways to help settle your stomach:
- Place a cool, damp cloth on your face.
- Take some slow, deep breaths.
- Take small sips of cold water or suck on ice chips (always check with your health-care team).
- Try distracting yourself with music or watching TV.
Eating, drinking, and digestion
Every person’s recovery is different. After surgery, your body needs healthy foods with extra calories and protein to help you heal. It is normal for your bowels to move slower than normal days or weeks after surgery.
After surgery, drinking and eating as soon as you can will help your bowels return to normal. Due to nausea or a lack of appetite, you may not feel hungry after surgery. Try eating smaller, more frequent meals, focusing on foods with higher protein.
The care team will monitor your blood sugar after surgery to ensure there are no unexpected changes/rises in blood sugar levels. Your body’s stress response can cause it to rise temporarily. If this occurs, insulin can be used to lower the blood sugar right after surgery.
Activity and exercise
It is important for you to get up and move around as soon as you can. Lying in bed leads to muscle weakness and can cause blood clots and lung infections.
Sternal precautions
Depending on the type of surgery you have, most people will have a sternotomy - a cut along the chest and through the sternum (breastbone). The sternum is then held together with stainless steel wires that stay in place long-term. After a sternotomy, the breastbone will take two to three months to heal. During this time, you must follow sternal precautions which include:
- No lifting anything weighing more than five to 10 pounds.
- Avoiding pushing or pulling with your arms.
- Hugging your chest when coughing.
Potential complications
Your surgeon and health-care team will discuss and review the most common complications with you in preparation for your surgery. Below are some common complications that cardiac surgery patients may experience.
-
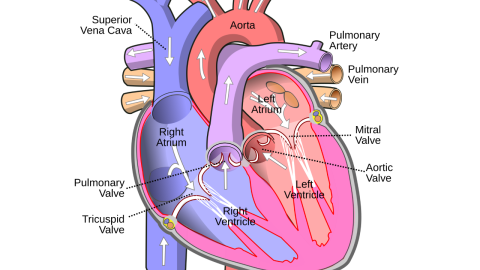
Atrial Fibrillation and Atrial Flutter
-
Atrial fibrillation/atrial flutter is a heart rhythm that often occurs after cardiac surgery due to the combined effects of having heart surgery.
-
Your health-care team will be monitoring you for this, which is one of the reasons that you wear the portable heart monitor after surgery.
- Patients say that fatigue and palpitations (the sensation that the heart is beating fast or irregularly) are the most common symptoms when experiencing atrial fibrillation.
- If you experience this heart rhythm, your surgeon and health-care team will usually treat it with medications (e.g. heart rate-controlling medications and blood thinners).
-
-
Post-Operative Delirium
- Delirium is a sudden change in your mental state that causes confusion.
- Delirium commonly occurs in older adults and people with serious or chronic medical conditions. Other risk factors may include alcohol withdrawal, lack of sleep, poorly managed pain, infections, some medications, or dehydration.
- Patients experiencing delirium may be sleepy, hard to wake up, restless or combative. They may also see or hear things that are not really there.
- Delirium is a medical condition that usually improves by treating the underlying cause.
- Your health-care team understands that delirium can be scary and will ensure you are safe and comfortable. They will answer any questions your family members may have and encourage their involvement in your recovery.
-
Pneumonia
- Pneumonia is an infection that inflames the air sacs in one or both lungs.
- The air sacs may fill with fluid or pus, causing a cough, phlegm, mucous, or pus, as well as fever, chills, and difficulty breathing.
- A variety of organisms, including bacteria and viruses, can cause pneumonia.
- Deep breathing and coughing exercises (ICOUGH) may help to prevent pneumonia.
-
Stroke
- A stroke can occur when there is not enough blood passing through the brain.
- This can occur when you bleed in one of the brain's blood vessels or when a blood clot prevents blood from passing through.
- Symptoms of stroke include facial drooping to one side, numbness or weakness in one arm, a sudden inability to speak properly, and/or blurred vision in one eye.
- Your surgeon assesses your risk of developing a stroke before surgery.
-
Dysphagia
- Having a breathing tube in your throat during surgery can irritate your throat and cause difficulty swallowing.
- Sometimes, a feeding tube through your nose will be needed to provide you with food, water and medications. This feeding tube will be removed when a swallowing test is done and you have passed and can safely swallow again.
- Some people may temporarily require a modified diet (food or fluid with a special texture) before they can safely swallow and resume a normal diet.
-
Blood transfusions
- In the event that you require a blood transfusion before, during or after your heart surgery, you will be asked to complete a consent form if you agree to receive blood
- Your surgeon will discuss specific indications for and risks of blood transfusions prior to surgery when you sign your surgical consent.
- If you require a transfusion, you must understand the risks of not getting a transfusion
- Canada’s blood system is among the safest in the world
- For more information, go to the Canadian Blood Services website: www.blood.ca
-
Effusions
- Pericardial effusion is the buildup of extra fluid in the sac (pericardium) around the heart. If too much fluid builds up, it can put pressure on the heart. This can prevent the heart from pumping normally.
- Pleural effusion is a collection of fluid in your chest around your lungs. If there is a large amount of fluid, your lungs may be unable to expand properly.
- If this happens, you may have the following symptoms:
- Chest/back/shoulder pain.
- Shortness of breath.
- Dizziness.
- Increased heart rate.
- Swelling in your arms and/or legs.
- Pain in the right upper abdomen.
- Nausea.
- Your health-care team will monitor you for these symptoms, but let them know if you experience any of these symptoms.
- If you experience this type of fluid buildup around your heart or lungs, you may need different medications or a small procedure to drain the fluid.
Important phone numbers
-
-
Cardiac Surgery Intensive Care Unit
If using an in-hospital phone, dial extension 54277.
-
Cardiac Sciences Acute Care Unit
Leon Blackmore 10th Floor (LB10A)
-