Your recovery in hospital after cardiac surgery: what to expect each day

Each person’s recovery is different. Depending on the type of surgery, most people are ready to go home in four to seven days.
Overview
| Activity | Tubes and lines | Pain medication | Food and nutrition | |
| Admission day (Day zero) day of surgery |
Surgery and bed rest |
Close monitoring in the ICU after surgery. |
IV |
No fluids |
| Day one after surgery |
Sit up. Take a short walk |
Heart monitor | IV / Oral | Fluids and food as tolerated |
| Day two after surgery |
Sit in a chair for meals and walk with help | Heart monitor | Less IV / Oral | Solid food, fluids |
| Day three after surgery |
Walking exercise |
Heart monitor |
Oral | Solid food, fluids |
| Day four after surgery |
Stairs with physiotherapy | Heart monitor, temporary pacemaker wire removed, confirm discharge | Oral | Solid food, fluids |
| Day five and beyond |
Going home | Discharge | Oral | Solid food, fluids |
Day of surgery (Day 0)
How will I feel?
- You will probably feel sleepy and need lots of rest.
- Your hands and legs may be swollen due to the IV fluids given during surgery.
What equipment do I have?
- Breathing tube.
- Oxygen mask, or nasal prongs.
- IV fluids.
- Catheter in your bladder to empty and measure the amount of urine.
- Dressing/bandage over your incision.
- Chest tube(s) to help drain fluid and air built up after surgery.
- Temporary pacemaker to help your heartbeat stay in steady rhythm.
*The breathing tube may be removed four to six hours after you come out of surgery
How is my pain treated?
-
Tylenol four times a day, IV opioids, other pain medications.
My activity goals:
- If you are stable and your care team has removed your breathing tube, get up to a chair or sit on the edge of the bed with help.
- Every hour while awake: Deep breathing and coughing exercises, leg exercises when in bed.
- Turn or change position in bed every two hours.
What can I eat?
When instructed by your health-care team, you may have a clear fluid diet. You may get medication to prevent or control nausea.
Can I wash?
We may help you wash in the evening.
Day one
How will I feel?
- You will probably feel less sleepy but will still need rest.
- Your hands and legs may be swollen due to the IV fluids given during surgery.
What equipment do I have?
- You may still have several pieces of equipment and tubes. Some of it may be removed.
- Intravenous (IV) line — we may leave it in place if you are not drinking liquids or if we are using it to give you medications.
- Chest tube(s).
- Catheter in your bladder.
- Temporary pacemaker to help your heartbeat.
- Portable heart monitor.
How is my pain treated?
Tylenol four times a day, IV opioids, other pain medications.
My activity goals:
- Get up to walk short distances with help.
- Sit up in a chair for all meals.
- Walk to the bathroom with help.
- Every hour while awake: Deep breathing and coughing exercises, leg exercises when in bed.
- Turn or change position in bed every two hours.
What can I eat?
- Eat or drink a regular diet or a diabetic diet (if you have diabetes).
- Drink enough fluids (as recommended by the health-care team) to prevent constipation. You may have fluid restrictions in place to prevent or manage fluid retention.
- You will receive medication for nausea if you need it.
- Let the nurse know if you pass gas or have a bowel movement.
Can I wash?
Yes, wash at your bedside or in the bathroom. You may need some help to set up.
Day two
How will I feel?
- You will start feeling stronger today.
- Rest between activities.
What equipment do I have?
- We may remove your intravenous (IV) line and urinary catheter.
- Chest tubes will be removed, if they haven’t been already.
- Portable heart monitor.
How is my pain treated?
Tylenol four times a day, opioids in pill form (less in IV form), and other pain medications if needed.
My activity goals:
- Get up into a chair with assistance.
- Sit up in a chair for all meals (minimum three).
- Walk to the bathroom with someone standing by.
- Every hour while awake: Deep breathing and coughing exercises, leg exercises when in bed.
- Turn or change position in bed every two hours.
- At least three times a day, walk around the unit with someone standing by.
What can I eat?
- Eat or drink a regular diet or a diabetic diet (if you have diabetes).
- Drink enough fluids (as recommended by the health-care team) to prevent constipation. You may have fluid restrictions in place to prevent or manage fluid retention.
- You will receive nausea medication if you need it.
- Let the nurse know if you pass gas or have a bowel movement.
Can I wash?
-
Yes, wash at your bedside or in the bathroom. You may need some help to set up.
Day three
How will I feel?
- You will feel stronger today. Continue to rest as required.
What equipment do I have?
- We may change or remove the dressing over your incision. You may see sutures or staples along the incision lines.
- Portable heart monitor.
- All other equipment and tubes may be removed or stopped.
How is my pain treated?
Tylenol four times a day and other pain medications if needed.
My activity goals:
- Sit up in a chair for all meals (minimum three).
- Walk to the bathroom without help.
- Every hour while awake: Deep breathing and coughing exercises, leg exercises when in bed.
- Turn or change position in bed every two hours.
- At least three to six times a day, walk around the unit on your own.
What can I eat?
- Eat or drink a regular diet or a diabetic diet (if you have diabetes).
- Drink enough fluids (as recommended by the health-care team) to prevent constipation. You may have fluid restrictions in place to prevent or manage fluid retention.
- Let the nurse know if you pass gas or have a bowel movement.
When can I go home?
You may be ready to go home in the next two days. Discuss your going home date with your health-care team.
Day four
How will I feel?
- You will feel stronger today. Continue to rest as required.
What equipment do I have?
- Your temporary pacemaker wires may be removed.
- Your sutures and/or staples may be removed.
-
Portable heart monitor.
How is my pain treated?
Tylenol four times a day and other pain medications if needed.
My activity goals:
- Sit up in a chair for all meals (minimum three).
- Walk to the bathroom without help.
- Every hour while awake: Deep breathing and coughing exercise, leg exercises when in bed.
- Turn or change position in bed every two hours.
- At least three to six times a day, walk around the unit on your own.
- Climb one flight of stairs.
What can I eat?
- Eat or drink a regular diet or a diabetic diet (if you have diabetes).
- Drink enough fluids (as recommended by the health-care team) to prevent constipation. You may have fluid restrictions in place to prevent or manage fluid retention.
- Let the nurse know if you pass gas or have a bowel movement.
Can I wash?
- You can have a shower today. Try not to let the water spray directly on your incisions.
When can I go home?
- You may be ready to go home tomorrow. Confirm plans for discharge and pick-up time with your health-care team.
- Arrange for someone to pick you up if you are going home tomorrow.
- Arrange for someone to pick up equipment from the Red Cross if recommended by the occupational therapist or physiotherapist.
-
Ensure you are registered for Fair PharmaCare.
Day five and until you leave hospital
How will I feel?
- You will feel stronger today. Continue to rest as required.
What equipment do I have?
- Sutures, staples, or temporary pacemaker wires will be removed if they haven’t been already.
- Your portable heart monitor will be removed.
How is my pain treated?
Tylenol four times a day and other pain medications if needed.
My activity goals:
- Sit up in a chair for all meals (minimum three).
- Walk to the bathroom without help.
- Every hour while awake: Deep breathing and coughing exercises, leg exercises when in bed.
- Turn or change position in bed every two hours.
- At least three to six times a day, walk around the unit on your own.
What can I eat?
- Eat or drink a regular diet or a diabetic diet if you have diabetes.
- Drink enough fluids (as recommended by the health-care team) to prevent constipation. You may have fluid restrictions in place to prevent or manage fluid retention.
- Let the nurse know if you pass gas or have a bowel movement.
Can I wash?
You can have a shower today. Try not to let the water spray directly on your incisions.
When can I go home?
- Confirm plans for discharge and pick-up time with your health-care team.
- Before you go home:
- Arrange for someone to pick you up if you haven’t already.
- Arrange for someone to pick up equipment from the Red Cross if recommended by the occupational or physiotherapist.
- Ensure you are registered for Fair PharmaCare.
- If you have questions, take time to ask us.
You are ready to go home when you meet the following criteria
- Your pain is managed with pills only.
- You can eat food with minimal discomfort.
- You are passing gas or have had a bowel movement.
- You can do simple self-care such as basic hygiene and walking short distances.
- Any problems after surgery are managed.
Leaving the hospital
During your hospital stay, you will receive discharge teaching. If you have questions, please ask your nurse. When you leave the hospital, you will be given a package containing important information.
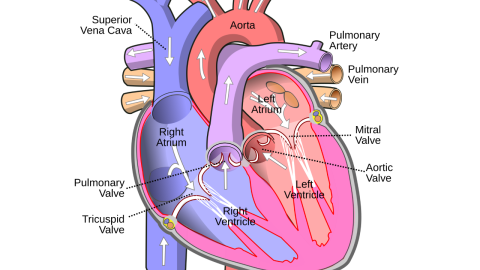
If you had Coronary artery bypass grafting (CABG) surgery, you will receive a diagram of your heart vessels that shows where the bypass grafts were placed.
If you had valve surgery, you will receive a temporary valve card: please keep this in your wallet. A permanent card will be mailed to your home in a few months.
Please bring this information to all your follow-up appointments.